As spring arrives we mustn't forget the potential hazards that our pets can encounter during the season.
CHOCOLATE
With lots of chocolate around the house, we'd like to remind pet owners, especially those with dogs, of the dangers of chocolate and the importance of keeping it out of reach.
The concentration of theobromine varies depending on the type of chocolate. For example, cocoa powder, baking chocolate and dark chocolate contain higher levels of theobromine compared to milk chocolate. The toxicity of theobromine is dose-related, meaning that the overall effect of chocolate ingestion on the dog depends on the size of the dog, the amount of chocolate eaten and the type of chocolate eaten.
The symptoms of theobromine ingestion may include restlessness, excitement, hyperactivity, nervousness, trembling, vomiting, diarrhoea, increased drinking and increased urination, increased heart rate, muscle tremors, seizures and possibly death.
If your dog (or cat) has ingested any chocolate (even a small amount) you should contact your vet immediately for advice.
Raisins/ sultanas/ grapes/ currants
It is unknown exactly why these foods are toxic to dogs, but it has been found that some dogs develop acute kidney failure following consumption of these fruits, even from eating a small amount. Hot cross buns are popular at Easter time, ensure that you keep them out of reach. It is important to contact your vet straight away should you suspect that your dog might have eaten any foods containing these fruits.
Other animals can potentially be affected too so keep these fruits and food containing these fruits out of the reach of all pets.
Lilies
A popular plant at this time of year, these beautiful flowers are best avoided if you have a cat in the household or you are giving flowers as a gift to a cat owner.
Lilies are poisonous to cats and can cause kidney failure. All parts of the plant are poisonous, even a small exposure to the pollen can be potentially very dangerous.
Contact us immediately if you suspect that your cat has come into contact with these flowers.
Garden safety
Cocoa mulch - This is often used in flower beds by gardeners but, as with chocolate, this contains theobromine which is poisonous to pets. Tree bark is a safer alternative.
Garden tools/equipment - Keep pets away from equipment during use. All garden tools should be returned to the shed or garage once they have finished being used, so that a pet doesn't accidently injure itself on their sharp points and edges.
Remember to check for wildlife such as hedgehogs and frogs before starting up the lawn mower or strimmer. Use a soft broom to brush through long grass and check under bushes on the edge of borders.
Fences and gates - Ensure that your garden perimeter is secure to prevent your dog escaping. Check for any gaps under the fencing and holes in the panels that they could venture through. Make sure that the fence is at a suitable height to prevent your dog jumping over it. Check that gate latches are functioning and gate locks are used for added security. Keep an eye on your dog whilst they are out in the garden as sadly dog thefts from gardens are on the increase.
Shed and garages - Check inside your shed and garage before closing the door as some cats are inquisitive and like to explore these buildings.
Flowers/plants - Many plants can pose a risk to pets if eaten. Some plants are more poisonous than others. You can find lists on the internet of pet-safe plants and those that are toxic and best avoided. While some pets aren't interested in nibbling plants, others are notorious for it. Puppies and kittens can be particularly prone to chewing - be sure to choose pet-safe plants with these pets. Supervision is also important. Fencing flower borders can help to stop dogs wandering into them.
Bulbs can look especially tempting, keep them out of reach.
Ponds - Take extra care if you have a pond in the garden. There are safety measures that can be put in place such as pond covers or fencing to create a barrier, or restrict access of your dog to the area.
Keep garden chemicals stored securely and out of reach of pets and children.
Ensure that they are used according to label instructions and keep your pet off of treated areas.
When selecting a product for purchase, and when using a product, read the label carefully as it will give clear and precise instructions regarding children and pets.
Slug bait - With showers and warm weather bringing out the slugs and snails, some gardeners are tempted to reach for the slug bait to protect their plants from these pests.
Metaldehyde is a common ingredient of slug pellets and is extremely poisonous. Pets are attracted to the cereal based pellets and will eat them. Pets that have consumed metaldehyde may become unsteady on their feet and become twitchy, this can then progress to convulsions and respiratory failure. If you have any concerns that your pet may have consumed any slug and snail pellets, call your vet ( or nearest vet to you) immediately - even if they appear well.
There are some newer slug and snail pellets available that do not contain metaldehyde. It is important to follow instructions on the packet and take precautions when using them. We would advise that if your pet was to accidentally eat them to contact your vet immediately for advice.
The best thing for a household with pets is to avoid using these products. There are alternatives to using slug pellets such as crushed egg shells, sand paper, slug pubs and copper tape/rings.
Fertilisers can also upset pets as the very high levels of minerals can cause toxic imbalances. Some fertilisers also contain herbicides, pesticides and fungicides, which are all potential poisons.
Rat bait - If using rodent poisons discuss their use with a professional, use pet friendly alternatives where possible and ensure that any bait is completely inaccessible to any pets. If accidental ingestion is at all expected contact your vet immediately. Not all rodenticides are the same so it is important to provide the vet with information on what was used.
OUT AND ABOUT
Identification - Some cats become more active this time of year and spend longer outside exploring, so make sure that your cat is micro-chipped. Call us to book an appointment!
It is a legal requirement for all dogs in the UK to be micro-chipped, so make sure that your dog is chipped.
Once a pet is microchipped it is imperative that your pet's details are registered to the microchip database. This is usually completed by the owner and can be done online or by post - follow your vet's advice. Once a pet is registered the database company will send you confirmation of registration.
It is important that your contact details on the microchip database are kept up to date.
Dogs must also wear a collar with a tag.
The tag should provide details of the owner.
We would NOT recommend to put your dog's name on the tag. Some owners choose to have the words ' I'm chipped ' engraved.
Walks - Check the fit and closure of collars, harnesses and leads.
Ensure your dog's collar is the correct fit - not too tight that it is uncomfortable and not too loose that it slips off over your dog's head. The rule of thumb says you should be able to get two fingers between the collar and the dog's neck.
There are many different types of harness available - research before you buy. It is important to measure your dog to ensure the harness fits correctly.
- Always keep your dog on a lead around wildlife and in fields where there are livestock. Also keep your dog on a lead if walking beside roads.
As the weather warms up, ensure that you carry water with you so that you can give your dog a drink.
Avoid leaving your dog tied up outside a shop - sadly pet theft is on the increase and unattended dogs can be a target for thieves.
Spring temperatures can fluctuate. What starts out as a cloudy day can soon turn into a glorious sunny afternoon. A parked car quickly heats up to a dangerous temperature - never leave your pet in a car.
Also be aware that conservatories and greenhouses quickly heat up to unbearable temperatures. Never leave your pet shut in a conservatory. Make sure that you check your greenhouse before closing the door just in case an animal has wandered inside.
RABBITS AND GUINEA PIGS
Don't be tempted to bring them out of their sheltered winter accommodation too soon, although the days are mild, the nights can get cold. Settle for a day run in the garden if the weather is nice until the night temperatures rise.
New fresh spring grass can be particularly rich for small tummies and you should introduce them to it gradually. Start with a small amount at a time ( allow them 10 minutes grazing time for example, increasing slowly over several days). Monitor their droppings to ensure they aren't soft.
NEVER feed grass clippings to your pet. The fermented clippings will make them ill.
As we enter into the warmer spring months, ensure that you provide your pets with adequate shelter from the sun.
Make sure that you keep their hutch in top-notch condition. Your pet will be happier and healthier and their home will be less appealing to flies.
Check your pets twice a day to ensure that bottoms are clean and dry. A dirty rear end can attract flies leading to a life threatening condition called flystrike. Flies lay their eggs, most commonly on the rear end, and the maggots that hatch attack the skin causing extensive damage. It is mostly seen in rabbits but it is a good idea to check guinea pigs too.
If you spot a dirty bottom, do speak to your vet as there is often an underlying cause that can be addressed such as diet, teeth issues, weight, arthritis.
Disclaimer :The contents of the Arden House Animal Hospital website are for informational purposes only. The content is not intended to be a substitute for professional veterinary advice, diagnosis, or treatment. Always seek the advice of your Veterinary Surgeon with any questions you may have regarding your animal’s medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website

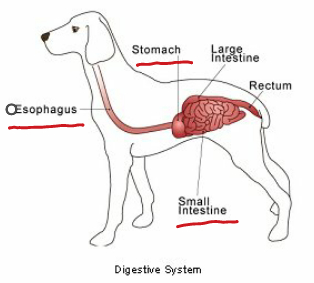 inside. Lotte required an operation called an exploratory laparotomy which involves making a surgical incision into the abdominal cavity in order to examine the abdominal organs and look for a foreign body. Vet Nigel, along with the assistance of a nurse, gave Lotte a general anaesthetic.Once Lotte was asleep, it gave Nigel the opportunity to fully examine Lotte's mouth. Looped around the base of Lotte's tongue was some wool and Nigel could see that both ends were extending down her oesophagus. Firstly Nigel cut the string from around the tongue and then Lotte was prepared for theatre. Nigel then carried out a procedure called a gastrotomy which involved making an incision into her stomach. This revealed more wool and Nigel could now access the string extending into the oesophagus. He carefully removed this via the opening in the stomach. Nigel could see that more wool had continued to make its way out of Lotte's stomach and into her small intestine.The next stage of the operation was to remove the wool from the length of the small intestine, a procedure called an enterotomy. Nigel carefully followed the wool along the small intestine and cut and removed it at four seperate incision sites. He found the free end of wool and finally it was all removed. All of the incision sites were then stitched and Lotte's operation was complete. Lotte was recovered from the anaesthetic and she was monitored closely in recovery by our nurses.Lotte was well enough to go home the following day. We are so pleased that lovely Lotte is now fully recovered.
inside. Lotte required an operation called an exploratory laparotomy which involves making a surgical incision into the abdominal cavity in order to examine the abdominal organs and look for a foreign body. Vet Nigel, along with the assistance of a nurse, gave Lotte a general anaesthetic.Once Lotte was asleep, it gave Nigel the opportunity to fully examine Lotte's mouth. Looped around the base of Lotte's tongue was some wool and Nigel could see that both ends were extending down her oesophagus. Firstly Nigel cut the string from around the tongue and then Lotte was prepared for theatre. Nigel then carried out a procedure called a gastrotomy which involved making an incision into her stomach. This revealed more wool and Nigel could now access the string extending into the oesophagus. He carefully removed this via the opening in the stomach. Nigel could see that more wool had continued to make its way out of Lotte's stomach and into her small intestine.The next stage of the operation was to remove the wool from the length of the small intestine, a procedure called an enterotomy. Nigel carefully followed the wool along the small intestine and cut and removed it at four seperate incision sites. He found the free end of wool and finally it was all removed. All of the incision sites were then stitched and Lotte's operation was complete. Lotte was recovered from the anaesthetic and she was monitored closely in recovery by our nurses.Lotte was well enough to go home the following day. We are so pleased that lovely Lotte is now fully recovered.










